Travel Vaccines
Travel vaccines, also known as travel immunizations or travel shots, are recommended or required for individuals traveling to specific destinations. These vaccines protect travelers from infectious diseases that might be more prevalent in certain regions. They help reduce the risk of contracting and spreading diseases that travelers might be exposed to during their journeys.
Importance of Travel Vaccines:
- Disease Prevention: Traveling exposes individuals to new environments and potential health risks. Travel vaccines protect against diseases that might be uncommon or even eradicated in one’s home country but are prevalent in other parts of the world.
- Personal Health: Travel vaccines are essential to maintaining personal health while exploring new places. Travelers can significantly reduce their risk of becoming ill during or after their trips by staying up-to-date with recommended vaccines.
- Public Health: Vaccination protects the traveler and contributes to global public health efforts. It helps prevent the importation and spread of diseases across borders.
- Prevention of Outbreaks: Unvaccinated travelers can inadvertently carry diseases back to their home countries, potentially leading to outbreaks. By getting vaccinated, travelers protect not only themselves but also their communities.
- Entry Requirements: Some countries have specific vaccine requirements for entry. Proof of vaccination might be necessary to obtain a visa or enter certain countries.
- Travel Plans Uninterrupted: Falling ill during a trip can disrupt travel plans and lead to unnecessary stress and expenses. Vaccination reduces the likelihood of getting sick and helps ensure a smoother travel experience.
- Risk Reduction: Certain diseases can have severe consequences, such as hospitalization or death. Travel vaccines can significantly reduce the risk of such outcomes.
- Destination-Specific Protection: Travel vaccines are tailored to specific diseases in particular regions. The vaccines you need might differ based on your travel destinations.
- Peace of Mind: Being protected against vaccine-preventable diseases gives travelers peace of mind, allowing them to focus on enjoying their journeys rather than worrying about their health.
It’s important to note that travel vaccines should be taken in consultation with a healthcare provider or travel medicine specialist. These professionals consider your destination, travel itinerary, medical history, and current health status to recommend the appropriate vaccines and timing. Planning and getting vaccinated well before travel is crucial to ensure your immune system has time to build immunity and offer effective protection.
DISCLAIMER: Below are general guidelines, and the specific timing might vary based on your health situation and travel plans. It’s crucial to consult with a healthcare provider or travel medicine specialist to receive personalized advice and ensure you’re fully protected before your travel.
Travel Vaccine: TDAP Vaccine
TDAP vaccine is a routine vaccine covered by most commercial insurance. We do provide this vaccine through insurance. You can learn about other Travel clinic services we offer on this page.
What are the recommendations for the TDAP vaccine for different age groups?
If you’re an adolescent between the ages of 11 and 12. It’s time to consider the Tdap vaccine. This booster is valuable to your routine vaccinations, safeguarding you against three serious diseases.
Fret not if you’re beyond your teenage years and haven’t had a Tdap vaccine. The protection that the vaccine offers is not bound by age. It’s recommended for adults who haven’t received a Tdap vaccine before or need a booster dose, usually every ten years.
What happens if you are contracted with Tetanus, Diphtheria, or Pertussis?
Tetanus: Accidents can happen anywhere, and Tetanus – the ‘lockjaw’ disease – is a potential risk. Tdap protects you against the bacteria that cause this painful and potentially fatal condition.
Diphtheria: This respiratory disease might feel like a distant memory, but its threat is real. Tdap protects your defenses against this contagious and sometimes severe illness.
Pertussis (Whooping Cough): Especially crucial if you’ll be around infants or young children. Pertussis can be severe for them. Your Tdap vaccine helps create a protective barrier, reducing the risk of transmission.
What is the side effect of the TDAP vaccine?
Tdap can have mild side effects, as with any vaccine, usually within a day or two. These might include a sore arm, slight fever, or mild discomfort – temporary signs that your immune system is responding.
Severe reactions are exceedingly rare, and allergies are even rarer. Discussing your concerns about past vaccine reactions or allergies with your healthcare provider is wise.
If you’re pregnant, the Tdap vaccine can be an extra shield for you and your baby. It’s often recommended during pregnancy to help safeguard against pertussis.
What is the cost of the TDAP vaccine, and where can I get it?
You can get the TDAP vaccine cost by visiting our book online link. The prices will be shown at the end of the booking flow after you select the date and time of the appointment. We provide the TDAP vaccine through insurance as it is a routine primary care vaccine. We do provide it as cash pay as well.
What country travel needs the TDAP vaccine?
The Tdap vaccine (Tetanus, Diphtheria, Pertussis) is often recommended for travelers to various countries, especially if they haven’t received a Tdap vaccine in the past ten years, or if they haven’t been vaccinated against pertussis (whooping cough) as adult. The Tdap vaccine is generally a routine recommendation for adults in many countries to maintain protection against these diseases.
Some countries might also recommend the Tdap vaccine for certain travelers based on their health status, activities, or potential exposure risks. For example, if you’re traveling to a country where you’ll be in close contact with infants or young children, getting vaccinated against pertussis can help prevent transmission to these vulnerable populations.
Travel Vaccine: COVID-19 Vaccine
The COVID-19 vaccine is the modern-day armor against the novel coronavirus that has reshaped the world. It’s been designed to help your immune system recognize and fight off the virus should you be exposed, reducing the severity of the illness or preventing it altogether. You can learn about other Travel clinic services we offer on this page.
Who should get vaccinated with COVID-19 vaccine?
The good news is that most countries are making COVID-19 vaccines available to everyone eligible. Whether you’re a seasoned traveler, a business explorer, or an adventure enthusiast, getting vaccinated can provide a shield of protection against the virus.
What can happen if you get contracted with COVID-19?
The vaccine offers you a personal layer of protection against severe illness and complications associated with COVID-19. It’s your way of fortifying yourself against the virus’s impact, ensuring that health concerns don’t derail your travel plans. Getting vaccinated also contributes to a wider community immunity, helping reduce the spread of the virus and protecting those who might be more vulnerable.
What are the different types of COVID-19 Vaccines:
Various COVID-19 vaccines have been developed and authorized around the world. Some require multiple doses for full efficacy, while others offer strong protection after one shot. Our team will guide you on which vaccine is recommended for your travel plans.
What are the potential Side Effects of COVID-19 vaccines?
As with any vaccine, COVID-19 can trigger mild side effects, often signaling that your immune system is responding as intended. These might include a sore arm, fatigue, mild fever, or body aches. These side effects are usually short-lived.
Why do you think the travel consultation is important for COVID-19 vaccine?
Our travel clinic is here to address your questions and concerns. We’ll provide guidance tailored to your needs if you have underlying health conditions or unique travel circumstances. Pre-travel consultations ensure you’re informed and confident about your decision.
What is the cost of Covid vaccine, and where can I get it?
Covid is a vaccine available in most pharmacies and some clinics. You can call your pharmacy and schedule your covid vaccination.
Travel Vaccine: Rabies vaccine
The Rabies vaccine is a defense against a virus often associated with animals but can pose a significant risk to humans if contracted. This vaccine protects you from the potentially fatal consequences of a Rabies infection. You can learn about other travel clinic services we provide on this page.
Rabies is a viral disease that can be transmitted to humans through the bite or scratch of an infected animal. While various animals can potentially transmit rabies, some animals are more commonly associated with transmitting the virus. The animals that are most frequently implicated in transmitting rabies to humans include:
Dogs: Dogs are a common source of rabies transmission in many parts of the world. Stray or unvaccinated dogs can carry the virus and transmit it to humans through bites.
Bats: Bats are known carriers of the rabies virus. Even a minor scratch or bite from a bat can transmit the virus. In some cases, individuals might not even be aware of the contact with a bat, as their bites can be very small and not easily noticed.
Raccoons: In some regions, raccoons can carry rabies and transmit it to humans. This is more common in North America.
Skunks: Skunks are another potential source of rabies transmission, particularly in regions where they are prevalent.
Foxes: In certain areas, foxes can carry and transmit rabies to humans.
Cats: While rabies transmission from cats is less common than from dogs, it’s still possible if a cat is infected.
Other Wild Animals: In some cases, other wild animals, like coyotes, mongooses, and jackals, can also carry and transmit rabies.
It’s important to note that the risk of rabies transmission varies by region and the prevalence of the virus in local animal populations. The best way to prevent rabies is to avoid contact with potentially infected animals, vaccinate pets against rabies, and seek immediate medical attention if you’re bitten or scratched by an animal, especially in areas where rabies is endemic. If there’s any suspicion of rabies exposure, post-exposure prophylaxis (PEP) should be administered promptly to prevent the development of the disease.
Who Should Consider the Rabies Vaccine?
The Rabies vaccine is especially important if your travel plans involve outdoor activities, wildlife encounters, or exploring rural areas where access to medical care might be limited.
The vaccine protects if your journey extends longer, increasing your chances of potential animal exposure.
Those involved in activities that bring them into contact with animals or potentially Rabies-infected material should also consider the vaccine.
What can happen if you contract Rabies?
Rabies is a viral disease transmitted through the saliva of infected animals, most commonly through bites. The vaccine prepares your immune system to combat the virus effectively should you be exposed, reducing the risk of severe illness. If you receive the Rabies vaccine before exposure, the treatment protocol after a potential exposure is simplified and less invasive, potentially saving you from undergoing Rabies immune globulin injections.
How many doses of Rabies vaccine are administered?
The Rabies vaccine is often given as a series of shots. Our travel clinic team will provide a recommended schedule based on your travel plans and potential exposure risks. We administer intra-muscular shots of Imovax vaccine from Sanofi Pasteur.
Pre-exposure dosage
As per the Advisory Committee of Immunization Practices, taking three doses of Rabies vaccine on day 0, day 7, and day 21 or 28 to gain immunity to the virus is recommended.
Post-exposure dosage for unvaccinated individual
Previous unvaccinated individuals should get five doses of Imovax vaccines on day 0, day 3, 7, 14 and 28 or later. Rabies immune globulin (RIG) should also be administered in full calculated dose to infiltrate the wound(s) on Day 0, along with the first vaccine dose. If unable to infiltrate, administer any remaining portion of the dose intramuscularly at a different site from the vaccine.
Post-exposure dosage for vaccinated individual
When a person previously vaccinated or demonstrated rabies antibody is exposed to rabies, they should receive two doses of Imovax Rabies vaccine, one immediately after exposure and one 3 days later. Rabies immune globulin (RIG) is not necessary in these cases. If the immune status of a previously vaccinated person who did not receive the recommended HDCV regimen is unknown, full primary post-exposure anti-Rabies treatment (RIG plus 5 doses of HDCV) may be necessary. In such cases, if antibody levels greater than 1:5 dilution can be demonstrated in a serum sample collected before vaccine is given, treatment can be discontinued after at least two doses of HDCV. (20)
What are the potential side effects of Rabies vaccine?
As with any vaccine, mild side effects can occur, including soreness at the injection site, mild fever, or fatigue. These effects are usually short-lived and minor compared to the potential risks of Rabies.
How can you safeguard yourself from Rabies for your travel adventures ahead?
Whether hiking in remote landscapes, engaging in wildlife-related activities or simply exploring areas with higher Rabies prevalence, the Rabies vaccine is a vital safeguard.
Consult our travel clinic to assess your specific travel plans, potential exposure, and personal health considerations. We’ll tailor our recommendations to ensure your health remains a priority.
As you gear up for your travel escapades, remember that your safety is paramount. The Rabies vaccine is your tool to mitigate potential risks and confidently enjoy your journey.
What countries travel needs Rabies vaccine?
Recommended for travelers to regions where rabies is prevalent, especially if activities involve close contact with animals. Areas where rabies is prevalent, particularly if you’ll be in close contact with animals. This might include countries like India, Thailand, Vietnam, and parts of Central and South America.
Who should not take the Rabies vaccine?
Individuals with severe allergies to any vaccine component. The vaccine is generally considered safe for most people.
How much time before should I take Rabies (Imovax) vaccine before my travel?
The rabies vaccine usually requires multiple doses over several weeks. Consult your healthcare provider for the recommended schedule based on the specific rabies vaccine.
What is the cost of the Rabies vaccine, and where can I get it?
We keep the rabies vaccine as a cash-pay service. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Yellow Fever Vaccine
The Yellow Fever vaccine is more than just a shot; it’s your shield against a viral disease that can have serious health consequences. This vaccine ensures that the threat of Yellow Fever doesn’t compromise your travel plans. You can learn about other Travel clinic services we offer on this page.
Who Should Consider the Yellow Fever Vaccine?
If you’re journeying to areas where Yellow Fever is endemic or where the disease is a known risk, the vaccine is a travel essential.
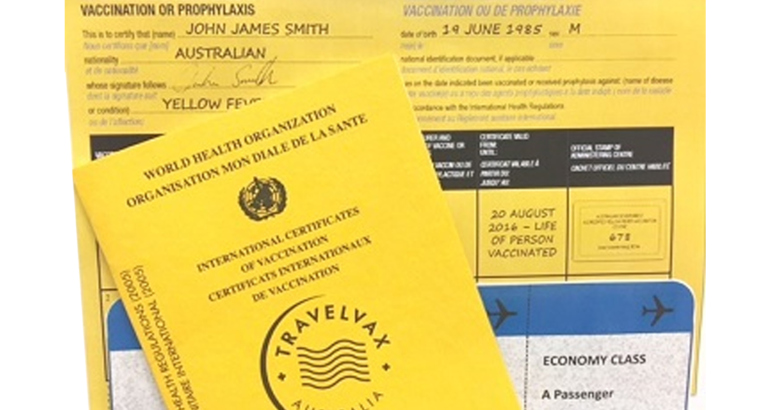
Some countries require proof of Yellow Fever vaccination for entry. Our travel clinic team can guide you on whether this requirement applies to your destination.
What can happen if we don’t take the Yellow Fever vaccine?
Mosquitoes transmit Yellow Fever, leading to severe symptoms, including high fever, jaundice, and even organ failure. The vaccine empowers your immune system to recognize and combat the virus, protecting you from harm.
How is the Yellow Fever vaccine administered?
The Yellow Fever vaccine is usually given as a single dose. The World Health Organization (WHO) recommends that this one-time vaccination provides lifelong protection.
What are the potential side effects of the Yellow Fever vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site, low-grade fever, or fatigue, can occur. These effects are transient and minor compared to the protection the vaccine offers.
Why is a Yellow Fever vaccine consult important?
Before you embark on your journey, consult our travel clinic to discuss your itinerary and the Yellow Fever risk associated with your destination. This conversation ensures that you’re well-informed and adequately prepared.
Whether you’re exploring the depths of tropical rainforests or strolling through vibrant urban centers in endemic regions, the Yellow Fever vaccine is your gateway to uninterrupted adventures.
Remember, preparation is the cornerstone of a safe and enjoyable journey. Partner with us to ensure that your health remains your greatest travel companion.
Who should not take the Yellow Fever vaccine?
Individuals with severe allergies to any vaccine component, infants younger than 6 months, pregnant or breastfeeding women (unless travel to high-risk areas is unavoidable), and individuals with certain immune system disorders.
What precautions to take for the YF vaccine?
Individuals with weakened immune systems or certain medical conditions might need to consult a healthcare provider before receiving the vaccine.
What countries travel are recommended Yellow Fever Vaccine?
Recommended for travelers to certain countries in sub-Saharan Africa and tropical South America where yellow fever is endemic. Countries might require proof of yellow fever vaccination for entry. Sub-Saharan Africa and tropical South America include Brazil, Nigeria, the Democratic Republic of Congo, Peru, etc. Some countries might require proof of yellow fever vaccination for entry, even if you’re passing through certain regions.
How long before I need to take this vaccine before my travel?
Ideally, you should receive the yellow fever vaccine at least ten days before traveling to a yellow fever-endemic area to ensure your body has enough time to develop immunity.
What is the cost of the Yellow Fever vaccine, and where can I get it?
We keep the Yellow Fever vaccine as a cash-pay service. We bill insurance for the yellow fever vaccine if your insurance covers it. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Meningitis vaccine
The Meningitis vaccine isn’t just about prevention; it’s about safeguarding yourself against a potentially devastating bacterial infection. This vaccine empowers you to explore without unnecessary health concerns. You can learn about other Travel clinic services we offer on this page.
Who should consider the Meningitis vaccine?
Travelers to High-Risk Areas: If you plan to journey to regions where Meningitis outbreaks are known to occur or are near the local population, the Meningitis vaccine is a valuable shield.
If your travels involve group settings, such as festivals, camps, or crowded events, the risk of Meningitis transmission can be elevated. The vaccine provides an added layer of protection.
Why does the Meningitis vaccine matter?
Protecting Brain Health: Meningitis is an infection that can lead to brain and spinal cord inflammation, causing severe symptoms and complications. The vaccine prepares your immune system to counter the bacteria responsible for this infection.
How is Meningitis Vaccine administered?
Menactra is administered as a 0.5 mL intramuscular injection. Children aged 9-23 months receive a 2-dose series three months apart. Individuals aged 2-55 receive a single dose. A booster dose can be given to those aged 15-55 if at continued risk for meningococcal disease, at least four years after the prior dose.
What is the potential side effect of the Meningitis vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site, mild fever, or fatigue, might occur. These effects are typically short-lived and minor compared to the potential risks of Meningitis.
Who Should not take the Meningitis vaccine?
Individuals with severe allergies to any vaccine component.
How long before I should take this vaccine before my travel?
The timing for the meningococcal vaccine can vary based on the specific type of vaccine used. Consult your healthcare provider for the recommended schedule.
What is the cost, and where can I get it?
We keep the meningitis vaccine as a cash-pay service. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Typhoid vaccine
Who should consider the Typhoid vaccine?
The Typhoid vaccine is your ally if your journey takes you to areas where Typhoid fever is prevalent due to unsanitary conditions or contaminated food and water. Your exposure to contaminated food or water might increase if you plan to explore local cuisines or dine in markets. The vaccine helps mitigate this risk. You can learn about other Travel clinic services we offer on this page.
Why does the Typhoid vaccine matter?
Typhoid causes fever caused by a bacterium found in contaminated food and water. It can lead to severe symptoms, including high fever and gastrointestinal distress. The vaccine primes your immune system to counter this threat.
What types of Typhoid vaccines are available?
The Typhoid vaccine is available in two forms: an injectable and oral. Our travel clinic team will discuss the most suitable option for your travel plans.
What are the potential side effects of the Typhoid vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site or low-grade fever, can occur. These effects are transient and minor compared to the potential risks of Typhoid fever.
What countries have Typhoid vaccine as a recommendation?
Recommended for travelers to regions with poor sanitation and hygiene practices, including parts of Asia, Africa, and Latin America. In Asia, Africa, and Latin America, sanitation and hygiene might be inadequate. Examples include India, Pakistan, Bangladesh, and various countries in Africa and South America.
Who should not take Typhoid vaccines?
Individuals with severe allergies to any vaccine component.
What precautions to take for this vaccine?
Individuals with weakened immune systems might need to consult a healthcare provider before receiving the vaccine.
How long before I need to take this vaccine before my travel?
The injectable typhoid vaccine should ideally be taken at least 2 weeks before travel. The oral typhoid vaccine (Ty21a) requires a series of doses taken over several days, so you might need to start it earlier.
What is the cost, and where can I get it?
We keep the Typhoid vaccine as a cash-pay service. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: HPV vaccine
While the HPV vaccine isn’t exclusive to travel, it aligns with our philosophy of prioritizing your well-being. By taking this step, you’re nurturing your health for a lifetime of journeys and experiences. Many developed countries include the HPV vaccine in their adolescent immunization programs. This is typically done to protect against HPV infections before individuals become sexually active and are potentially exposed to the virus. The HPV vaccine is often recommended for individuals between 9 and 26. The optimal age for vaccination can vary based on local guidelines and the vaccine used. You can learn about other Travel clinic services we offer on this page.
Who should consider the HPV vaccine?
Adolescents and Young Adults: The HPV vaccine is recommended for adolescents and young adults to protect against human papillomavirus (HPV) infections. These infections can lead to various cancers later in life.
Why the HPV vaccine matters?
HPV is a common virus transmitted through sexual contact. While most HPV infections resolve independently, some can lead to serious health issues, including cervical, anal, and oropharyngeal cancers. The vaccine helps prevent these potential complications.
How is the HPV vaccine administered?
The HPV vaccine is typically administered as a series of shots. The number of doses and the schedule depend on the age at which you start the vaccine series.
What are the potential side effects of this vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site, mild fever, or fatigue, can occur. These effects are transient and minor compared to the potential benefits of HPV protection.
What is the cost, and where can I get it?
Currently, we are not administering the HPV vaccine, but our clinic can do the consult and provide you with a vaccine order for the HPV vaccine. You can get this vaccine from any of the pharmacies.
Travel Vaccine: Meningococcal vaccine
As a travel clinic, we ensure your travels are exciting but safe and well-informed. You can learn about other Travel clinic services we offer on this page.
Who Should Consider the Meningococcal Vaccine?
If your journey takes you to regions where Meningococcal disease outbreaks are known to occur, the vaccine becomes a crucial part of your travel preparations. If your travels involve large gatherings, dormitories, or crowded places where close contact is common, the risk of Meningococcal transmission might increase. The vaccine offers an added layer of protection.
What can happen if the Meningococcal vaccine is not taken?
Meningococcal disease can lead to severe symptoms, including high fever, headaches, and even life-threatening complications. The vaccine readies your immune system to fight off the bacteria responsible for this disease.
How is the Meningococcal vaccine administered?
The Meningococcal vaccine comes in different types, each targeting specific strains of the bacteria. Our travel clinic team will guide you on the most suitable vaccine for your travel itinerary.
What are the potential side effects of the Meningococcal vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site, mild fever, or fatigue, can occur. These effects are usually short-lived and minor compared to the potential risks of Meningococcal disease.
What country travel needs the Meningococcal vaccine?
Recommended for travelers to the “meningitis belt” in sub-Saharan Africa, where meningococcal disease is more common. Sub-Saharan Africa’s “meningitis belt,” which stretches from Senegal in the west to Ethiopia in the east. This belt includes Mali, Niger, Burkina Faso, and Sudan.
What is the cost, and where can I get it?
We keep the Meningococcal vaccine as a cash-pay service. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Hepatitis B vaccine
Who should consider the Hepatitis B vaccine?
If your travels span multiple countries or regions, the risk of exposure to Hepatitis B can vary. The vaccine becomes a key consideration in your travel health strategy. If your journey involves long-term stays, whether for work or leisure, your potential exposure to the virus might increase. The vaccine provides an added layer of protection. Hepatitis B vaccine is a routine vaccine covered by most commercial insurance. We do provide this vaccine through insurance. You can learn about other Travel clinic services we offer on this page.
Why does the Hepatitis B Vaccine matter?
Defending Against Hepatitis B: Hepatitis B is a viral infection that attacks the liver and can lead to chronic health issues. The vaccine ensures your immune system is primed to thwart the virus, safeguarding your well-being.
How is Hepatitis B vaccine administered?
The Hepatitis B vaccine is usually given in a series of shots. The number of doses and the schedule depend on the vaccine formulation and your specific health needs.
What is the potential side effect of the Hepatitis B vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site, mild fever, or fatigue, can occur. These effects are transient and minor compared to the potential risks of Hepatitis B infection.
What countries travel has Hepatitis B vaccine recommendation?
Recommended for travelers to countries with intermediate to high rates of hepatitis B infection, such as parts of Asia, Africa, and some areas in Eastern Europe. Regions with intermediate to high rates of hepatitis B infection. This can include parts of Asia, Africa, and Eastern Europe. Examples include China, Philippines, Nigeria, and Romania.
Who should not take the Hepatitis B vaccine?
Individuals with severe allergies to any vaccine component.
How long before I should take this vaccine before my travel?
The hepatitis B vaccine is typically administered in a series of three doses over a period of several months. The second dose is usually given one month after the first, and the third dose is given six months after the first.
What is the cost, and where can I get it?
We keep the hepatitis B vaccine as a cash-pay service. We do bill insurance for this vaccine if they cover it. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Hepatitis A vaccine
If you are traveling to multiple countries or regions, your risk of exposure to Hepatitis A may vary. Getting vaccinated should be a key consideration in your travel health strategy, especially if you are staying long-term for work or leisure. The Hepatitis A vaccine is covered by most commercial insurance and we offer it at our Travel clinic, along with other services. You can check our extensive Travel clinic services here.
Who should consider the Hepatitis A vaccine?
If your travels take you across international borders, the risk of exposure to Hepatitis A can vary. The vaccine becomes a vital component of your travel health strategy.
If you’re eager to savor local cuisines or indulge in street food, your exposure to contaminated food and water might increase. The vaccine provides an extra layer of safety.
What can happen if you contract Hepatitis A?
Defending Against Hepatitis A: Hepatitis A is a viral infection that primarily affects the liver and can cause severe symptoms. The vaccine primes your immune system to fight off the virus, protecting your health.
How is the Hepatitis A vaccine administered?
The Hepatitis A vaccine is typically administered in two doses for long-term protection. Our travel clinic team will guide you on the appropriate schedule.
What is the potential side effect of the Hepatitis A vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site, mild fever, or fatigue, can occur. These effects are temporary and minor compared to the potential risks of Hepatitis A infection. Areas with poor sanitation and hygiene practices, including many developing countries worldwide. Examples include Mexico, India, Egypt, and various countries in Southeast Asia.
What travel country has recommendations of Hepatitis A vaccines?
Recommended for travelers to areas with inadequate sanitation and hygiene practices, including many developing countries worldwide.
Who should not take Hepatitis A vaccine?
Individuals with severe allergies to any vaccine component.
How long before I should take Hepatitis A vaccine before my travel?
A single dose of the hepatitis A vaccine provides some protection, but for long-term immunity, you should ideally receive the second dose 6 to 12 months after the first.
What is the cost, and where can I get it?
We keep the Hepatitis A vaccine as a cash pay service. We also bill insurance for this vaccine if it is covered by insurance. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Japanese Encephalitis Vaccine
This vaccine guards against a viral infection transmitted by mosquitoes in parts of Asia. This illness can lead to brain inflammation and severe complications. The vaccine reduces the risk of contracting this serious disease by building immunity. It’s crucial for travelers to high-risk areas, especially those planning long-term stays. The vaccine is typically given in two doses and is suitable for all ages, with mild side effects like soreness or fever. Consultation with our travel clinic ensures the best vaccination plan for your journeys. With this vaccine, you can explore with confidence and safety. You can look at the extensive list of travel clinic services at this page.
Who should consider the Japanese Encephalitis vaccine?
If your journey takes you to rural or agricultural areas of Asia, particularly during the transmission season of the virus, the Japanese Encephalitis vaccine is a wise consideration.
If your travel itinerary includes outdoor activities like hiking, camping, or exploring rice paddies, where mosquito exposure might be elevated, the vaccine becomes even more relevant.
What can happen if you contract Japanese Encephalitis?
Japanese Encephalitis is a viral infection transmitted by mosquitoes. It can lead to inflammation of the brain and severe neurological complications. The vaccine prepares your immune system to counter this potential threat.
How is the Japanese Encephalitis vaccine administered?
The Japanese Encephalitis vaccine is typically administered in two doses, with a time gap between doses. This vaccine requires proper planning due to the schedule involved, so consulting our travel clinic well in advance is advised.
What is the recommended age group for the Japanese Encephalitis vaccine?
The vaccine is recommended for individuals two months and older, especially those in high-risk areas.
What is the potential side effect of the Japanese Encephalitis vaccine?
As with any vaccine, mild side effects, such as soreness at the injection site, mild fever, or fatigue, can occur. These effects are temporary and minor compared to the protection the vaccine offers.
What country travel needs the Japanese Encephalitis Vaccine?
Recommended for travelers to rural areas of Asia, particularly during the transmission season of the virus. Rural areas of Asia, particularly during the transmission season of the virus. Countries might include parts of India, Southeast Asia, and East Asia.
Who should not take the Japanese Encephalitis Vaccine?
Individuals with severe allergies to any vaccine component. Individuals with severe allergies to gelatin or a previous vaccine dose might need to consult a healthcare provider before receiving the vaccine.
How long before I should take this vaccine before my travel?
The Japanese encephalitis vaccine is typically administered in a series of two doses. The second dose is usually given 28 days after the first.
What is the cost, and where can I get it?
We keep the Japanese Encephalitis vaccine as a cash pay service. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Cholera Vaccine
The Cholera vaccine protects against a waterborne bacterial infection that leads to severe diarrhea and dehydration. It’s recommended for travelers heading to areas with cholera outbreaks or inadequate sanitation. The vaccine helps reduce the risk of infection and its consequences. Depending on the type, the vaccine may require multiple doses. While mild side effects can occur, the benefits of protection outweigh them. Consult our travel clinic to determine if the Cholera vaccine is appropriate for your journey. With this vaccine, you can venture with greater peace of mind. You can look at the list of travel clinic services at this page.
Who should consider the Cholera vaccine?
If your journey takes you to regions with ongoing cholera outbreaks or where cholera is endemic, the vaccine should be on your radar.
The vaccine is especially relevant if your travel plans involve remote areas, disaster relief work, or humanitarian efforts where access to clean water and sanitation might be compromised.
What can happen if the Cholera vaccine is not taken?
Cholera is a bacterial infection transmitted through contaminated food and water. It leads to severe diarrhea and dehydration. The vaccine primes your immune system to fight off the bacteria responsible for this disease.
How is Cholera administered?
The Cholera vaccine is often provided in a series of doses, usually administered orally. Timing and dosage may vary depending on the specific vaccine formulation.
What is the recommended age group for the Cholera vaccine?
The vaccine is generally recommended for individuals aged 2 years and older.
What is the potential side effect of the Cholera vaccine?
Like any vaccine, mild side effects, such as temporary stomach upset or mild diarrhea, might occur. These effects are short-lived and minor compared to the protection the vaccine offers.
What country travel needs the Cholera vaccine?
Recommended for travelers to areas with ongoing cholera outbreaks or endemic cholera, particularly in regions with inadequate sanitation and clean water access. Areas with ongoing cholera outbreaks or endemic cholera include regions in Africa, Asia, and parts of the Caribbean and South America.
Who should not take the Cholera vaccine?
Individuals with severe allergies to any vaccine component. The vaccine is generally considered safe for most people.
How long before I should take this vaccine before I travel?
The cholera vaccine (Vaxchora) is a single-dose oral vaccine that should ideally be taken at least 10 days before potential cholera exposure.
What is the cost, and where can I get it?
We don’t administer this vaccine at our clinic, but our doctor can prescribe this vaccine which you can take at a nearby pharmacy.
Travel Vaccine: Tick-Borne Encephalitis Vaccine
The Tick-Borne Encephalitis vaccine guards against a viral infection transmitted by ticks in certain parts of Europe and Asia. This illness can lead to brain inflammation and neurological complications. The vaccine builds immunity and reduces the risk of infection. It’s crucial for travelers exploring wooded or grassy areas in high-risk regions. Typically given in multiple doses, the vaccine offers protection for various age groups. Mild side effects may occur. Consultation with our travel clinic ensures proper vaccination planning. With the Tick-Borne Encephalitis vaccine, you can explore nature with confidence and safety. You can check our travel clinic services on this page.
Who should consider the Tick-Borne Encephalitis vaccine?
Explorers of Forested Areas: If your journey takes you to regions with dense forests and potential tick exposure, particularly in parts of Europe and Asia, the TBE vaccine should be on your radar.
Outdoor Enthusiasts: If your travel itinerary includes camping, hiking, or exploring nature reserves, where tick encounters might be elevated, the vaccine becomes especially relevant.
What is Tick-Borne Encephalitis?
Borne Encephalitis is a viral infection transmitted by ticks. It can lead to inflammation of the brain and severe neurological complications. The vaccine prepares your immune system to counter this potential threat.
How is the Tick-Borne Encephalitis vaccine administered?
The Tick-Borne Encephalitis vaccine is usually provided in a series of doses. The schedule may involve multiple doses and booster shots depending on the vaccine type.
What is the recommended age group for the Tick-Borne Encephalitis vaccine?
The vaccine is typically recommended for individuals aged one year and older traveling to high-risk areas.
What country travel needs the Tick-bone encephalitis vaccine?
Recommended for travelers to certain forested regions of Europe and Asia, where tick-borne encephalitis virus is present. Forested regions of Europe and Asia where tick-borne encephalitis virus is present. This might include countries like Russia, Central, and Eastern Europe, and some parts of China.
Who should not take the Tick-bone encephalitis vaccine?
Individuals with severe allergies to any vaccine component. The vaccine is generally considered safe for most people.
How long before should I take this vaccine before I travel?
The timing for the tick-borne encephalitis vaccine can vary based on the specific vaccine used. Consult your healthcare provider for the recommended schedule.
What is the cost, and where can I get it?
We keep the Tick borne encephalitis vaccine as a cash-pay service. You can check the prices using the book online button and schedule an appointment by calling the clinic.
Travel Vaccine: Flu shot / Influenza vaccine
The Flu vaccine safeguards against seasonal influenza viruses that cause respiratory illness. It’s recommended annually for people of all ages, especially those at higher risk. The vaccine reduces the chance of getting the flu and its complications. Available in various formulations, including shots and nasal sprays, the vaccine is tailored to different age groups. Mild side effects like soreness or low-grade fever might occur. Consult our healthcare experts for personalized guidance. With the Flu vaccine, you can face flu season with resilience and health. You can have a look at our travel clinic services on this page.
Who should consider the Flu shot?
If your journey falls during the flu season at your destination or transit points, getting the Influenza vaccine is a wise choice.
You’re at greater risk of flu complications if you have underlying health conditions or weakened immunity. The vaccine becomes even more crucial in protecting your health.
What happens if you get Flu?
Influenza, or the flu, is a highly contagious respiratory illness. The vaccine readies your immune system to fight off the circulating strains of the virus, reducing your risk of infection.
How is the Flu shot vaccine administered?
The Influenza vaccine is an annual shot, as the strains of the flu virus can change yearly. It’s usually available ahead of the flu season.
What is the recommended age group for the Flu shot vaccine?
The Influenza vaccine is recommended for individuals of all ages, especially those at higher risk of flu-related complications, such as young children, the elderly, and people with chronic health conditions.
What are the potential side effects of Flu shot vaccine?
As with any vaccine, mild side effects such as soreness at the injection site, low-grade fever, or fatigue might occur. These effects are transient and minor compared to the potential risks of the flu.
What country travel needs a Flu shot vaccine?
Recommended for travelers to various regions, especially during the flu season, as strains can differ between countries. Worldwide, depending on the flu season and the strains in circulation. It’s important to consider the timing and strains prevalent in your destination.
Who should not take the Flu shot vaccine?
Individuals with severe allergies to any vaccine component. Individuals with severe egg allergies might need to consult a healthcare provider before receiving the vaccine.
How long before I should get this vaccine before my travel?
The timing for the influenza vaccine depends on the flu season in your destination. It’s recommended to get vaccinated before the start of the flu season.
What is the cost, and where can I get it?
It is a routine vaccine that we give to our patients. We usually bill it to insurance if they cover it. You can call our clinic or visit our book online page to schedule a visit.
Travel Vaccines: Polio Vaccine
The Polio vaccine protects against the poliovirus, which causes polio, a paralyzing and potentially fatal disease. It’s crucial for travelers to regions where polio and those without prior vaccination are concerned. The vaccine boosts immunity and helps prevent the spread of the virus. It suits various age groups, administered in different forms, including injections and oral doses. Minor side effects like soreness can occur. Consult our healthcare experts for tailored advice. With the Polio vaccine, you contribute to global health efforts and a journey with greater safety. You can look at our extensive travel clinic services at this page.
Who should consider the Polio vaccine?
If your journey takes you to regions where polio is still a concern, especially areas with active outbreaks or endemic transmission, the vaccine should be on your checklist. If you’re committed to being part of the solution for a polio-free world, regardless of your destination, the vaccine gains an added significance.
What can happen if you contract Polio?
Polio, or poliomyelitis, is a highly contagious viral disease that can lead to paralysis and lifelong disability. The vaccine prepares your immune system to stand against the virus.
How is the Polio vaccine administered?
The Polio vaccine comes in two forms: the inactivated poliovirus vaccine (IPV) and the oral poliovirus vaccine (OPV). Depending on your destination and vaccination history, one or both may be recommended.
What is the recommended age group for the Polio vaccine?
The Polio vaccine is recommended for travelers of all ages, including adults. Sometimes, a booster dose might be recommended for adults who’ve completed their routine childhood polio vaccinations.
What are the potential side effects of the Polio vaccine?
The Polio vaccine is generally safe and well-tolerated. Common side effects include soreness at the injection site and mild fever. Serious side effects are extremely rare.
How long before I need to take the Polio vaccine before travel?
The timing for receiving the Polio vaccine before travel can vary based on the specific type of vaccine being used and your vaccination history. Here’s a general guideline for the timing:
Inactivated Poliovirus Vaccine (IPV):
If you’re not up-to-date with your routine polio vaccinations or need a booster dose, the IPV vaccine can be administered at any time before travel.
Oral Poliovirus Vaccine (OPV):
If you need the OPV vaccine, it’s usually recommended at least 4 weeks before travel. It’s important to note that the Polio vaccine is often part of routine childhood vaccinations, and many adults might already be vaccinated. In such cases, you might not need an additional vaccine dose for travel.
What is the cost, and where can I get it?
We provide polio vaccine as a cash-pay service. You can review prices and book appointments online using the book online button.
Travel Vaccines: Varicella vaccine
The Varicella vaccine shields against the varicella-zoster virus, preventing chickenpox and its complications. Recommended for susceptible individuals, especially travelers to areas with higher risk. The vaccine builds immunity and reduces the chance of infection. Given in two doses, it’s suitable for various age groups. Minor side effects like soreness and mild fever might occur. Consult our healthcare experts for personalized guidance. You can journey without worrying about chickenpox interrupting your plans with the Varicella vaccine. You can look at our other travel clinic services on this page.
Who should consider the Varicella vaccine:
If you haven’t had chickenpox or received the vaccine in childhood, and you’re traveling to areas where chickenpox is prevalent, the vaccine should be on your radar.
The Varicella vaccine becomes especially relevant for your travel health plan if you value minimizing the risk of common infectious diseases.
What happens if you get contracted with Varicella?
Varicella, commonly known as chickenpox, is a highly contagious viral illness. The vaccine prepares your immune system to fend off the virus and its potential complications.
How is the Varicella vaccine administered?
The Varicella vaccine is typically administered in two doses, with the second dose given a few weeks to a few months after the first.
What is the recommended age group for the Varicella vaccine?
The Varicella vaccine is recommended for susceptible adults who haven’t had chickenpox and are at risk of exposure during travel.
What is the potential side effect of the Varicella vaccine?
The Varicella vaccine is generally safe. Mild side effects might include soreness at the injection site, fever, and rash. Serious side effects are extremely rare.
What is the cost of this vaccine, and how can I book an appointment?
We provide this vaccine as a cash pay only vaccine. You can check the prices and book online using this page.